Vaginitis is one of the most common pathological conditions of the female reproductive system. It affects women of all ages and causes discomfort that leads the woman to the doctor.
How is it caused?
Ulcers occur as a result of a change in the balance of the microbial flora of the vagina.
When the lactobacilli that keep the vaginal environment acidic are reduced in number, the microbes of the vaginal flora prevail and cause inflammation.
What microbes are normally found in the vagina?
Vaginal microbiome or flora during reproductive age:
- 70 – 90% lactobacilli
- Gardnerella vaginalis (vaginal Haemophilus)
- E. coli
- Group B streptococci
- Genital mycoplasma
- Candida albicans
- Symptoms of vaginitis
- Vaginal discharge, often with an unpleasant odor
- Pain, itching or burning in the area
- Pain during intercourse
- Discomfort during urination
- Types and causes of vaginitis
- Non-specific vaginitis (BACTERIAL VAGINOSIS): Gardnerella vaginalis,
- Mycoplasma hominis, Anaerobic bacteria, Composite bacterial colonies (Biofilms)
- Trichomonas: Trichomonas vaginalis
- Candidiasis: Candida albicans, Candida krusei, Candida glabrata
Atrophic vaginitis (Genitourinary syndrome of menopause): - Estrogenopenia
- Exfoliative inflammatory vaginitis: No specific bacterium responsible has been identified. Almost total absence of lactobacilli.
- Allergic contact dermatitis: Contact irritation, allergic reaction with exacerbations
- Diabetes
Women with diabetes have more frequent vaginal yeast infections.
Diabetic women have increased glucose in their vaginal secretions, and since glucose is an excellent nutrient for fungi, they overgrow.
Preparation for the exam
Do not use vaginal creams two twenty-four hours before the examination.
Avoid sexual contact for 48 hours before your test.
Do not use tampons.
Avoid bubble baths in a full bathtub. Before your examination, showering is recommended.
How is the exam done?
You will be asked to remove your clothing from the waist down.
You lie in a comfortable examination chair, placing your legs in special supports so that they remain open during the sampling.
The doctor gently inserts the dilator into your vagina, causing only minimal discomfort.
The sample is taken by the doctor in special swabs and the dilator is removed.
Diagnosis
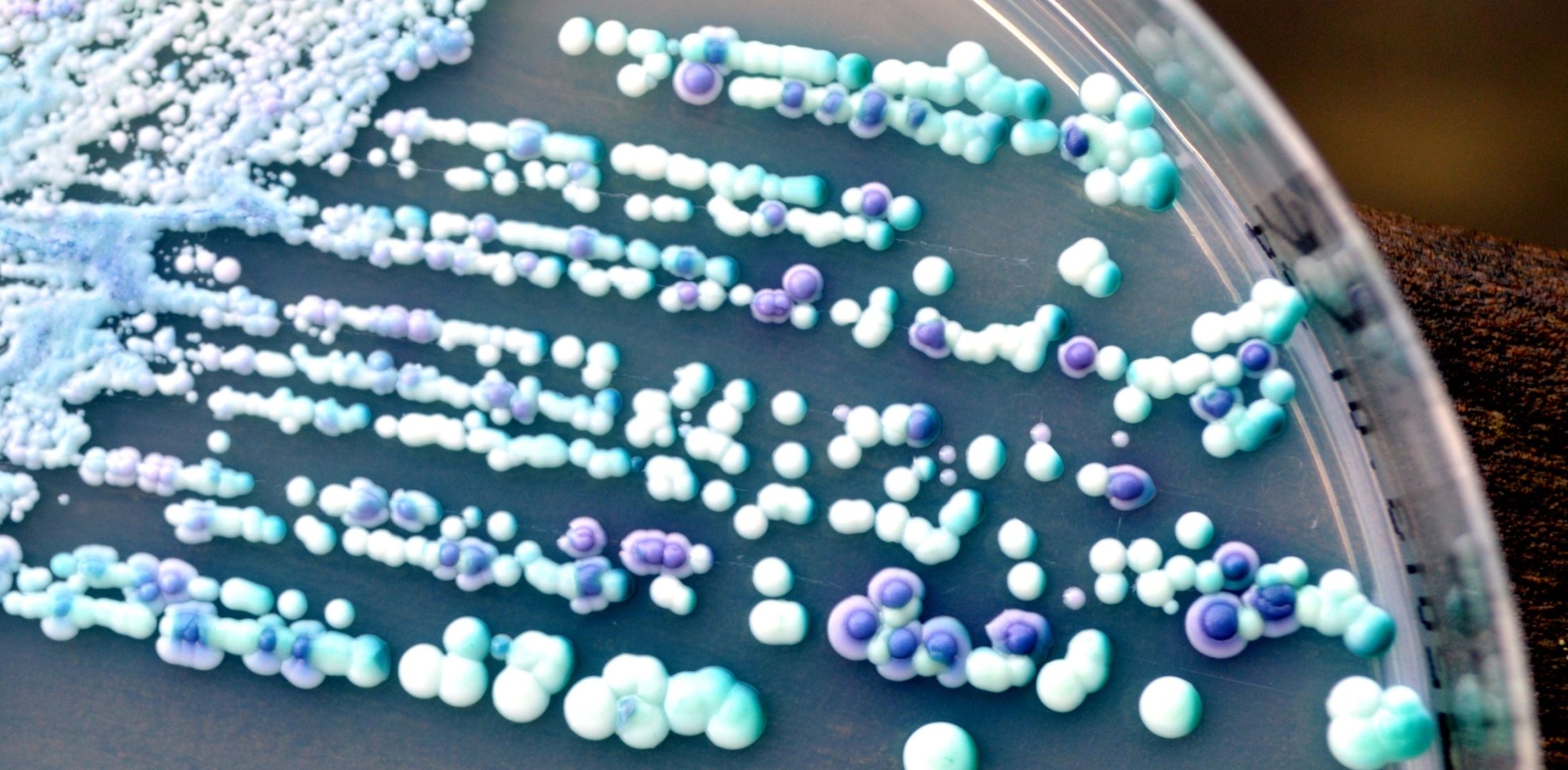
In the LabCare laboratories, a vaginal swab is taken by the doctor.
Direct preparation microscopy is then performed as well as smear microscopy after Gram staining.
In addition, aerobic and anaerobic micro-organisms and fungi are cultured.
A culture for chlamydia, mycoplasma, and ureaplasma is also performed (when the clinician suspects cervicitis).
An antibiogram is performed on a positive culture.
If requested, it is possible to check the vaginal microbiome with RT-PCR.
When will I get a result?
You will have results of the cultivation in three twenty-four hours.
Treatment
The type of treatment for ulcers depends on the factor that causes them.
Oral antibiotic or antifungal medications, vaginal creams and suppositories are the treatment, which should only be taken on the recommendation of your doctor and not empirically.
Prevention
Take good care of the hygiene of the area
Avoid using antiseptic soaps that disturb the vaginal flora.
Apply intravaginal washes only on the recommendation of your gynecologist.
Prefer cotton and loose pants and underwear as tight and synthetic ones create irritation due to friction and consequently disturbance of the vaginal microbiome.
Change your bathing suit after swimming in the sea or the pool, as the humidity favors fungal infections.
Do not use scented tampons.
Make sure you have safe sex. You will thus avoid forms of vaginitis caused by sexually transmitted bacteria.
For any medical issue that concerns us, we consult exclusively with our doctor!